Arthritis of the Shoulder
Shoulder arthritis is a problem without a great solution. Here are some of the variations and possibilities.

Shoulder pain can be due to soft tissue injuries (commonly the rotator cuff or the biceps tendon), wearing away of the articular cartilage at the head of the glenoid or the humerus (or glenohumeral joint, at the ball and socket of the shoulder), or at the acromial clavicular (AC) joint, where the collarbone meets the shoulder scapula. But unlike problems with the knee or ankle cartilage, wear in the shoulder has been nearly impossible to solve.
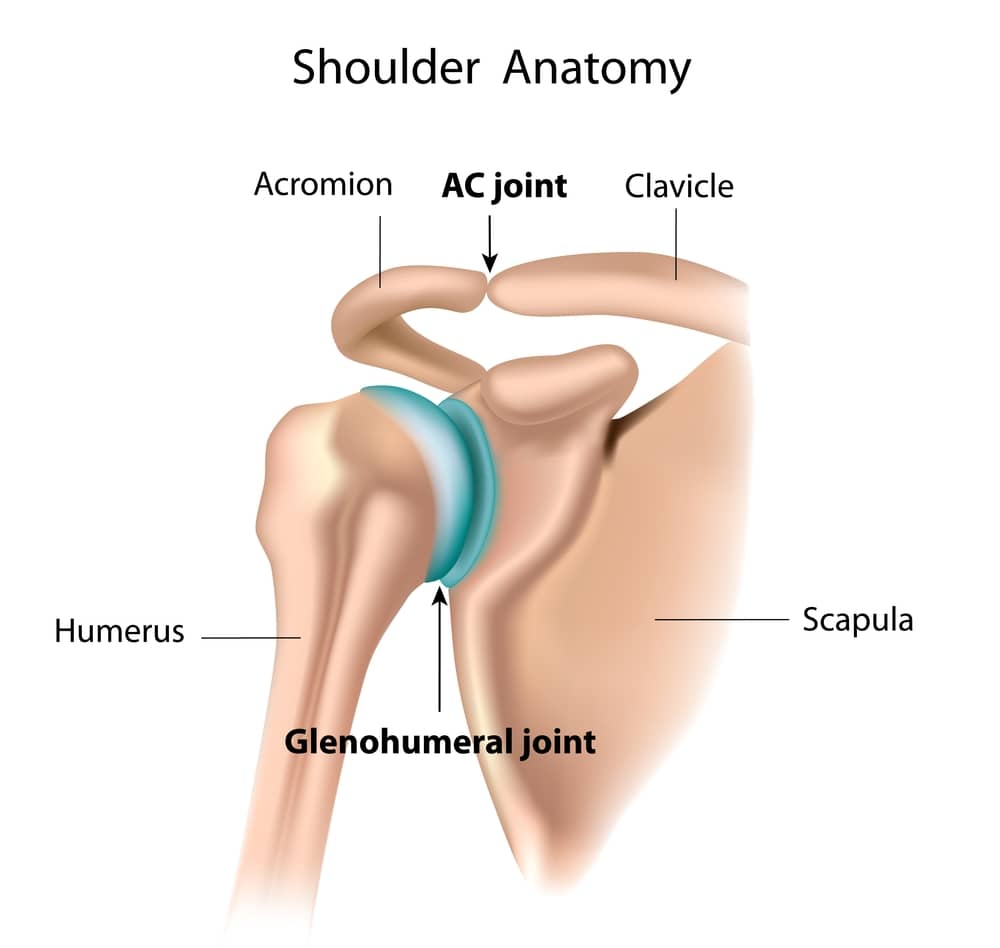
The reason for this is that the ball and socket joint formed by the humerus and glenoid do not respond well to the cartilage stimulation techniques we use elsewhere. This is in part because the shoulder cartilage is thin and the ball and socket require perfect congruence. Any rough area or divot leads to rapid additional erosion. Also, the biology of the shoulder cartilage is different from that of the knee and ankle. When fractured, smooth repair tissue does not form reliably.
The shoulder’s AC joint is also quite different. It is comprised of angular surfaces, confined to a tight space. When arthritic, the joint forms spurs (osteophytes) that dig into the underlying rotator cuff. This causes pain when the shoulder is elevated or during weight lifting. Many long-term weight lifters develop AC joint arthritis.
Early signs of shoulder arthritis are usually pain alone, as any swelling in the shoulder is hidden by the large muscles that surround it. Medical interventions are designed to prevent the progressive loss of motion that occurs in all arthritic joints. These strategies include stretching exercises and injections of lubrication (hyaluronic acid) and growth factors, including platelet-rich plasma (PRP). Cortisone is avoided due to its damaging effects on the tendons and suppression of normal cartilage cell metabolism.
Surgery for arthritis at the glenohumeral joint is problematic, as cartilage repair procedures have not worked reliably. Surgery to remove spurs and inflammatory tissue often helps for a while but is not curative. At the AC joint, removing the spurs and partially opening the joint—while maintaining its structural support—is one of the strategies for buying time. Full resection of the joint leads to later pain and instability.
Shoulder joint replacement with artificial components works well to relieve pain, but it has not been a pathway to full sports participation for many patients. Often the procedure is done late in the course of the disease, after the muscles have atrophied and the rotator cuff has degenerated or torn. This combination of disease states leads to poor function compared to a normal shoulder.
The future lies in our research, and that of others, to develop much more potent cartilage repair procedures so that arthritis is treated, prevented, and cured when possible. Today, the source of the compounds most likely to stimulate repair are birth tissues—the Wharton's Jelly surrounding the growing fetus, donated at the time of healthy Caesarean section. Nothing grows faster than the fetus and the anabolic components surrounding it. Those stem cells, progenitor cells, growth factors, and recruitment factors are anabolic, antifibrotic, and immunomodulatory. The fountain of youth, it turns out, is found in our most youthful. It can (and will) bring new healing strength to our aging bodies. Arthritis will meet its match.