What We Don’t Know About Stress Fractures
Stress fractures are injuries to bone that are frustrating to treat. Here is why:
Bone injuries can appear as frank fractures where the cortex (the outside edges of the bone) is broken, usually due to trauma. However, they can also appear as an injury inside the bone, involving the marrow or the spongy bone beneath the hard shell of the cortex. These injuries present in a range of ways and have a wide variety of treatments—which usually tells you there is no one best way to cure them.
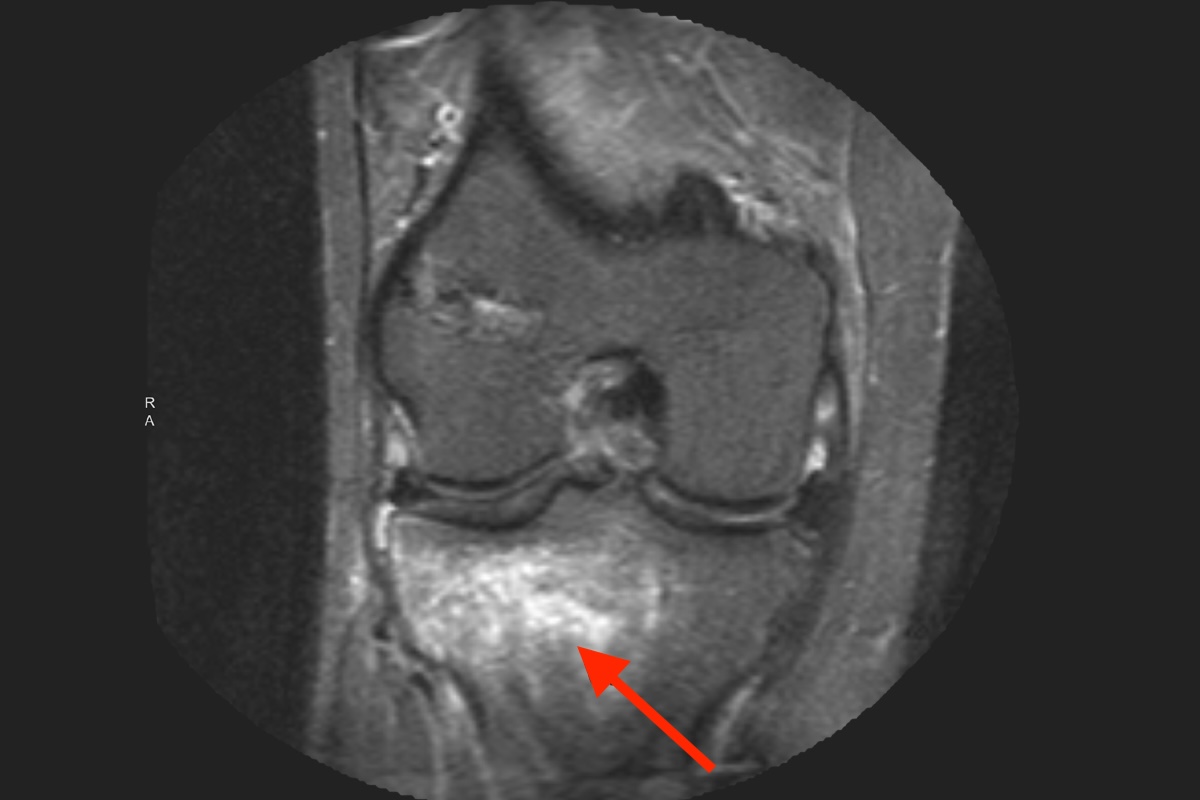
Bone injuries from overuse are classically reported by female runners who, in high school, have suddenly increased their mileage or returned from summer break and joined a track team or taken on a new sport involving jumping (especially if they were previously cyclists). They tell of new-onset pain that hasn’t gone away. The bones of the foot or shin are the most common injury sites. An X-ray is often normal. An MRI shows the classic white signal (highlighting fluid) within the otherwise dark bone. Both the coach and the athlete’s mom want to know how soon the patient can return to impact sports. Obviously, this story is repeated in athletes of all ages.
Bone injuries associated with more aggressive trauma, such as an ACL rupture, also show familiar patterns on an MRI. The diagnosis of an ACL tear can be made simply by looking at the bony signals on the MRI, though an exam is required to understand the degree of knee instability.
Bone injuries from relative osteoporosis are also common. The stress fracture of an adolescent with mild anorexia or a diet deficient in protein is one presentation. The stress fracture of an older person with significant inactivity or disease-generated osteoporosis is another.
The treatment of all stress fractures is controversial. The reason is that after an injury, the classic advice is to rest and let the body heal. Bone, however, responds to force by making more bone, while rest produces osteoporosis (weak bones). The key is to provide just the right amount of force, combined with a healthy diet and stimulation of natural healing hormones and marrow stem cells to accelerate the healing process.
Force-generating techniques include mild exercise, with bone loading of just the right amount. Electrical, ultrasound, shock wave, magnetic, and vibratory energy all stimulate the bone marrow cells, inducing them to produce more calcified collagen fibers (bone). Which device works best is unknown, but all seem to help heal stress fractures. The earlier these devices are applied the better, but unfortunately, insurance companies often make people wait months to determine whether or not the stress fracture will heal on its own.
We don’t know if injections of growth factors from PRP or marrow stem cells are helpful early in the disease, but we do inject them — with some encouraging results — for chronic fractures that have not healed.
All of the stimulatory methods above work best when the biology of the human body is optimized. This means, starting at the top, that the mind has to be in a positive framework (depression suppresses key hormonal stimulation for collagen production). The hormonal balance must not be off. Better yet, hormonal stimulation such as additional testosterone may be therapeutic. Nutrition plays a key role as levels of Vitamin D, Vitamin C, calcium, magnesium, and probably many others are vital to optimize the benefits of exercise and bone stimulation. Body mechanics play a role as well. Worn-out shoes, hard cement surfaces, and/or abnormal angles of body and foot alignment contribute to the overuse of one part of the anatomy versus another.
When a stress fracture occurs, a careful workup of all the potential factors and the institution of an immediate therapeutic program shorten the course and heal the bone. Delays create a disability that has ruined many a season for athletes of all ages. The “stress” in stress fracture can be contagious…But the opportunity to optimize the entire physical and mental program can also be a godsend.
